Critical Limb Ischemia

What is Critical limb ischemia?
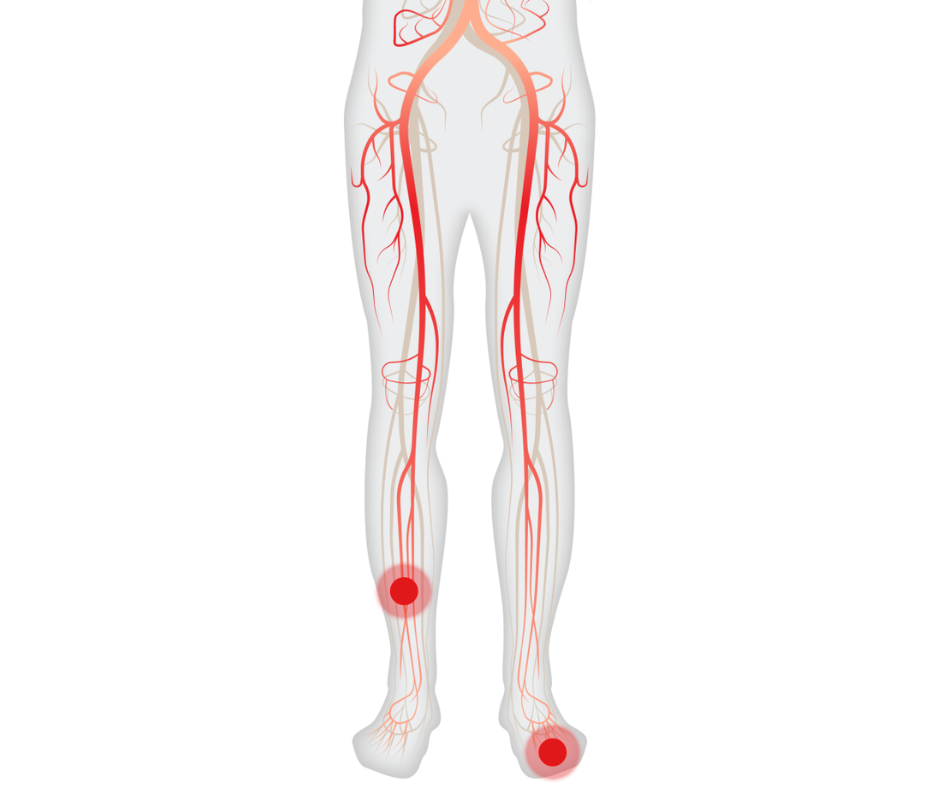
Critical Limb Ischemia (CLI) is a highly debilitating vascular condition characterized by a significant arterial obstruction, resulting in a marked reduction of blood flow to the extremities, namely the hands, feet, and legs. In advanced stages, CLI can lead to severe pain and the development of skin ulcers or sores. The pain experienced in CLI, known as “rest pain,” can interrupt an individual’s sleep and is typically localized in the leg. Temporary relief may be achieved by elevating the leg over the bed or engaging in light ambulation.
CLI represents an advanced manifestation of peripheral artery disease (PAD) and necessitates comprehensive intervention from a specialized vascular surgeon or vascular specialist. Spontaneous improvement of this condition is unlikely, emphasizing the importance of timely and appropriate medical management.
Critical limb ischemia is a severe stage of peripheral artery disease (PAD). Chronic critical limb ischemia presents with the clinical triad of rest pain, non healing wounds, and gangrene.
Critical Limb Ischemia Risk Factors:
Chronic critical limb ischemia is the end-stage consequence of arterial occlusive disease, primarily attributed to atherosclerosis. Common risk factors for this condition include hypertension, hypercholesterolemia, cigarette smoking, and diabetes. Less frequently, chronic critical limb ischemia can arise from Buerger’s disease (thrombo angiitis obliterans) or certain forms of arteritis.
Diabetes carries particular significance as a risk factor due to its strong association with severe peripheral arterial disease. Individuals with diabetes tend to develop atherosclerosis at a younger age, and the disease progresses rapidly in this population. Furthermore, atherosclerosis in diabetic patients primarily affects more distal vessels, such as the profunda femoris, popliteal, and tibial arteries, while the narrowing of the aorta and iliac arteries is relatively minimal. These distal arterial lesions pose challenges for effective revascularization procedures.
The combination of atherosclerosis in distal arteries and diabetic neuropathy contributes to the heightened rates of limb loss observed in diabetic patients compared to those without diabetes. The involvement of distal arteries, coupled with the neuropathic effects of diabetes, significantly increases the risk of limb complications in this patient population.
Critical Limb Ischemia Symptoms:
Chronic critical limb ischemia can manifest through various symptoms indicating a compromised blood supply to the legs and feet. These symptoms include:
- Severe pain or numbness experienced in the legs and feet while at rest or not moving.
- Noticeable decrease in temperature in the lower leg or foot compared to the rest of the body.
- Persistent sores, infections, or ulcers on the toes or feet that either do not heal or heal very slowly.
- Development of gangrene, which is characterized by tissue death and a blackened appearance.
- Skin on the legs or feet appearing shiny, smooth, and dry.
- Thickening of the toenails.
- Absent or diminished pulse in the legs or feet, indicating compromised blood flow.
Critical limb ischemia Diagnosis:
The identification of rest pain can present challenges when differentiating it from chronic leg pain associated with conditions like peripheral neuropathy. Additionally, determining whether a wound is non healing is subjective. However, there are several physical indicators and objective hemodynamic parameters that can support a diagnosis of chronic critical limb ischemia. Notable physical signs include the absence or reduction of pedal pulses, smooth and shiny skin on the feet and legs, and muscle wasting in the calves.
Objective assessment of blood flow can be easily conducted using a handheld Doppler probe and a blood pressure cuff. The cuff is inflated until the Doppler can no longer detect the pulse distal to the cuff. It is then slowly deflated until the pulse became audible again. This measurement is recorded as the systolic pressure. As mentioned previously, an ankle systolic pressure of 50 mm Hg or lower, or a toe systolic pressure of 30 mm Hg or lower, indicates the presence of critical limb ischemia.

The ankle-brachial index is another widely utilized parameter. It involves calculating the ratio of the systolic pressure at the dorsalis pedis or posterior tibial artery to the systolic pressure at the brachial artery. Patients with claudication typically exhibit an ankle-brachial index between 0.5 and 0.8, while those with critical limb ischemia generally have an ankle-brachial index of 0.4 or lower.
In vascular laboratories, Doppler probes are employed to measure the pulse volume waveform at various segments of the leg arteries. Changes in the Doppler waveform, progressing from triphasic to biphasic, monophasic, and eventually stenotic waveforms, can identify locations of arterial blockage.
Fontaine Classification for CLI:
I Asymptomatic
IIa Mild Claudication
IIb Moderate-severe claudication
III Ischemic rest pain
IV Ulceration or gangrene
There are other classifications as well for staging the Critical limb ischemia
Critical Limb Ischemia Treatment:
Critical limb ischemia treatment options are necessary to reduce the likelihood of amputation. Treatment options include medication to prevent clots and lower blood pressure and cholesterol, minimally invasive endovascular procedures like angioplasty or atherectomy, and surgical interventions using either natural veins or synthetic replacements. In cases where these treatments fail to restore blood flow, amputation of a portion of the affected limb may be necessary.
CLI is a major cause of amputation of legs. It’s very unfortunate outcome, But now it’s easily solved by increasing the vascular supply of legs. These leads to increase blood supply by 4 times so as to avoid unwanted amputation.
The management of refractory diseases requires a multidisciplinary approach aimed at discovering definitive solutions for improved quality of life. Recent advancements in regenerative medicine have opened doors for therapeutic angiogenesis using stem cells, recombinant proteins, and gene transfer.
Stem cells have gained attention as a promising therapeutic option for various conditions, including critical limb ischemia (CLI), due to their ability to promote angiogenesis and their regenerative and immunomodulatory effects on damaged tissues. Autologous bone marrow stem cells (a-BM-SC) have been considered the standard for limb ischemia treatment. However, this approach has limitations such as the common cardiovascular risk profile of CLI patients and complications associated with invasive procedures for cell extraction. Additionally, the angiogenic potential of transplanted cells is influenced by the donor’s characteristics, which may be compromised in CLI patients due to age and overall health. Hence, a-BM-SC may not be the optimal therapeutic choice for Critical . Alternative sources of stem cells have been explored to overcome these challenges. Mesenchymal stem cells (MSCs) have emerged as a particularly attractive option for CLI treatment. MSCs offer several advantages over other stem cell populations, including the ability to be derived from healthy allogeneic donors, low immunogenicity (reduced expression of MHC class II molecules), anti-inflammatory properties, and relative ease of in vitro expansion . These features have led to the development of preclinical and clinical trials for ischemic disorders such as stroke, coronary artery disease, and CLI. This review aims to highlight the characteristics, functions, and mechanisms of action of MSCs in the context of therapeutic angiogenesis for Critical limb ischemia.
Frequently Asked Questions
Critical limb ischemia (CLI) is a severe arterial blockage in the lower extremities, causing significantly reduced blood flow. It is a serious type of peripheral arterial disease (PAD), although less prevalent than claudication.
Your healthcare provider may suggest medications to prevent clots, lower blood pressure, and reduce cholesterol. They may also recommend minimally invasive endovascular treatments like angioplasty (with stent placement) to open blocked arteries or atherectomy to remove plaque buildup.Stem cell therapy has been one of the best treatment options for Critical Limb Ischemia
Prompt treatment is essential for critical limb ischemia to minimize the risk of amputation. Multidisciplinary management approaches are necessary for refractory diseases to find effective solutions and improve quality of life. Recent advances in regenerative medicine, such as therapeutic angiogenesis using stem cells, recombinant proteins, and gene transfer, have provided new opportunities for treatment.
Auscultation: Stethoscope confirms the presence of a “whooshing” sound (bruit) in leg arteries.
Ankle-brachial index (ABI): Ratio of arm and ankle systolic blood pressures.
Doppler Ultrasound: Measures blood flow direction and velocity in vessels.
CT angiography: Advanced X-ray generates 3D images.
MR angiography: Radiofrequency waves and magnetic fields create 2D and 3D vessel images.
Angiogram: X-ray study of blood vessels using contrast dyes.

