Knee Arthroscopy
Introduction
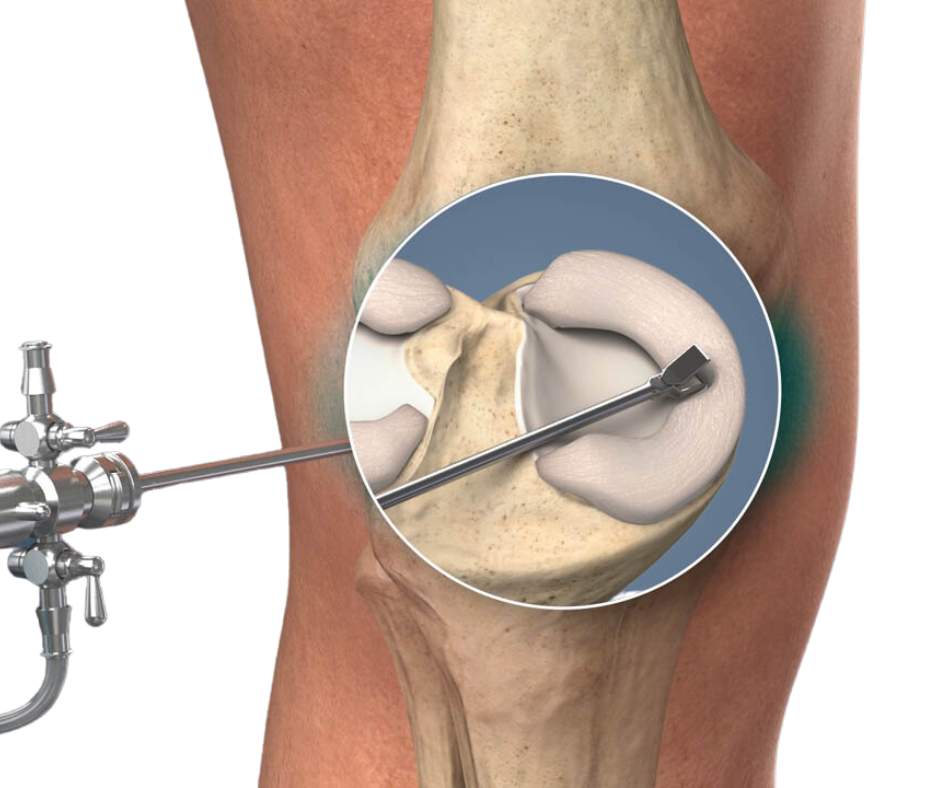
Knee arthroscopy, also known as knee scoping, is a minimally invasive surgical procedure used to diagnose and treat various knee conditions and injuries. This procedure involves the use of an arthroscope, a small surgical instrument equipped with a camera and light, to provide a clear view of the inside of the knee joint.
Understanding Knee Arthroscopy
Knee arthroscopy is typically recommended for patients who have not responded to nonsurgical treatments such as medication, cortisone injections, or physical therapy. It is particularly effective in addressing pain associated with cartilage damage or soft tissue injuries.
Compared to other procedures, knee arthroscopy offers several advantages. The surgeon only needs to make a small incision to insert the arthroscope, resulting in less pain, reduced joint stiffness, and a faster recovery time.
Indications for Knee Arthroscopy
Knee arthroscopy serves two main purposes: diagnosis and surgery. When used for diagnosis, the procedure allows the surgeon to view the inside of the knee and confirm the extent of the injury or condition. This is especially helpful when imaging tests, such as X-rays, do not provide sufficient information.
In surgical cases, additional incisions are made to accommodate the surgical tools alongside the arthroscope. With the guidance of the arthroscope’s images, the surgeon can repair torn ligaments, remove damaged meniscus, eliminate loose bone fragments, or perform other necessary treatments.
Preparing for Knee Arthroscopy
Before undergoing knee arthroscopy, a thorough preoperative assessment is essential. This includes a detailed medical history, physical examination, and evaluation of the patient’s airway, nutritional status, and current medications. Laboratory tests or an electrocardiogram (ECG) may be required based on the patient’s age or medical condition.
To alleviate anxiety, patients may be given midazolam or opioids. Reflux prophylaxis, such as a nonparticulate antacid, is recommended for patients with moderate-to-severe reflux or diabetic gastroparesis. Antibiotics, such as first-generation cephalosporins, may be administered as prophylaxis against common skin flora. For patients receiving neuraxial anesthesia, adequate intravenous hydration is crucial to reduce the risk of bradycardia and cardiac arrest.
Anesthesia Options for Knee Arthroscopy
The choice of anesthesia technique for knee arthroscopy depends on various factors, including patient preferences, comorbidities, surgeon and anesthesiologist preferences, and the complexity of the procedure. The available options include general anesthesia, neuraxial anesthesia, peripheral nerve blockade, and local anesthesia.
General anesthesia can be administered using a laryngeal mask airway (LMA) or endotracheal intubation. This technique is suitable for anxious patients and children. Different anesthetics, such as isoflurane, sevoflurane, or propofol with nitrous oxide, can be used depending on the desired recovery time and patient satisfaction.
Neuraxial anesthesia provides motor blockade and analgesia while allowing the patient to remain awake or lightly sedated during the procedure. The use of small-gauge, pencil-point needles can minimize the risk of postdural puncture headache (PDPH). Intrathecal opioids may be administered to enhance postoperative analgesia. Another option, epidural 3% 2-chloroprocaine, has shown promising results with minimal side effects.
Peripheral nerve blockade offers excellent analgesia, shorter post-anesthesia care unit (PACU) stays, and a low incidence of side effects. However, it can be time-consuming and may result in decreased patient satisfaction and prolonged motor blockade. Combining techniques, such as general anesthesia with local anesthesia or peripheral nerve block, may be suitable for certain patients but does not necessarily provide additional benefits for diagnostic procedures.


Anesthetic Management and Monitoring
Standard ASA monitors should be applied to all patients undergoing knee arthroscopy. Additional monitors may be necessary based on the patient’s medical condition. Proper positioning is crucial to avoid nerve injuries, and pressure points should be padded in both the upper and lower extremities.
Most knee arthroscopies can be performed in a semi-lithotomy position with slight flexion of the table. Tourniquet pain can be managed with intravenous opioids or sedation, along with reassurance. Anesthetics like propofol, midazolam, and fentanyl have relatively short durations of action. Fluid losses during the procedure are generally minimal, and a single intravenous line is usually sufficient.
Potential Complications and Postoperative Care
Although complications are rare, it is essential to be aware of potential risks associated with knee arthroscopy. These may include nausea and vomiting, sedation, back pain, PDPH, neuropathy, transient neurological syndrome, urinary retention, and hypotension. Surgical complications, such as pain, bleeding, infection, hemarthrosis, or the need for further surgery, may also occur.
Postoperative pain management options include intraarticular bupivacaine, peripheral nerve blocks, NSAIDs (e.g., ketorolac, ibuprofen), oral opioids, cryotherapy, or transcutaneous electrical nerve stimulation (TENS). Each patient’s pain management plan should be tailored to their specific needs.
In conclusion, knee arthroscopy is a valuable diagnostic and surgical tool for addressing various knee conditions and injuries. When performed under appropriate anesthesia, with careful monitoring and postoperative care, knee arthroscopy can lead to successful outcomes and improved quality of life for patients.
*[ASA]: American Society of Anesthesiologists
*[PACU]: Post-Anesthesia Care Unit
*[NSAIDs]: Nonsteroidal Anti-Inflammatory Drugs
*[TENS]: Transcutaneous Electrical Nerve Stimulation

